Public Health Concern Adverse Childhood Experiences (ACEs)
In the mid 1990’s Kaiser Permanente and the CDC did a large study (over 17,000 participants) to look at the relationship between childhood trauma and later medical problems. (1) This body of work known as Adverse Childhood Experiences (ACE) Study established that there was a significant impact on later health associated with the number of trauma types reported. The higher the ACE score the more significant the impact was. Furthermore, the study identified that 64% of respondents reported 1 or more types of traumas. Other later studies show that the impacts of exposure to childhood trauma are dose-dependent for a wide range of learning (2), behavioral and health problems in childhood (3,4) and adulthood health problems (5,6). Including Obesity, Diabetes, Ischemic heart disease (7), COPD (8) and cancer (9) all leading to increased risk of early mortality.
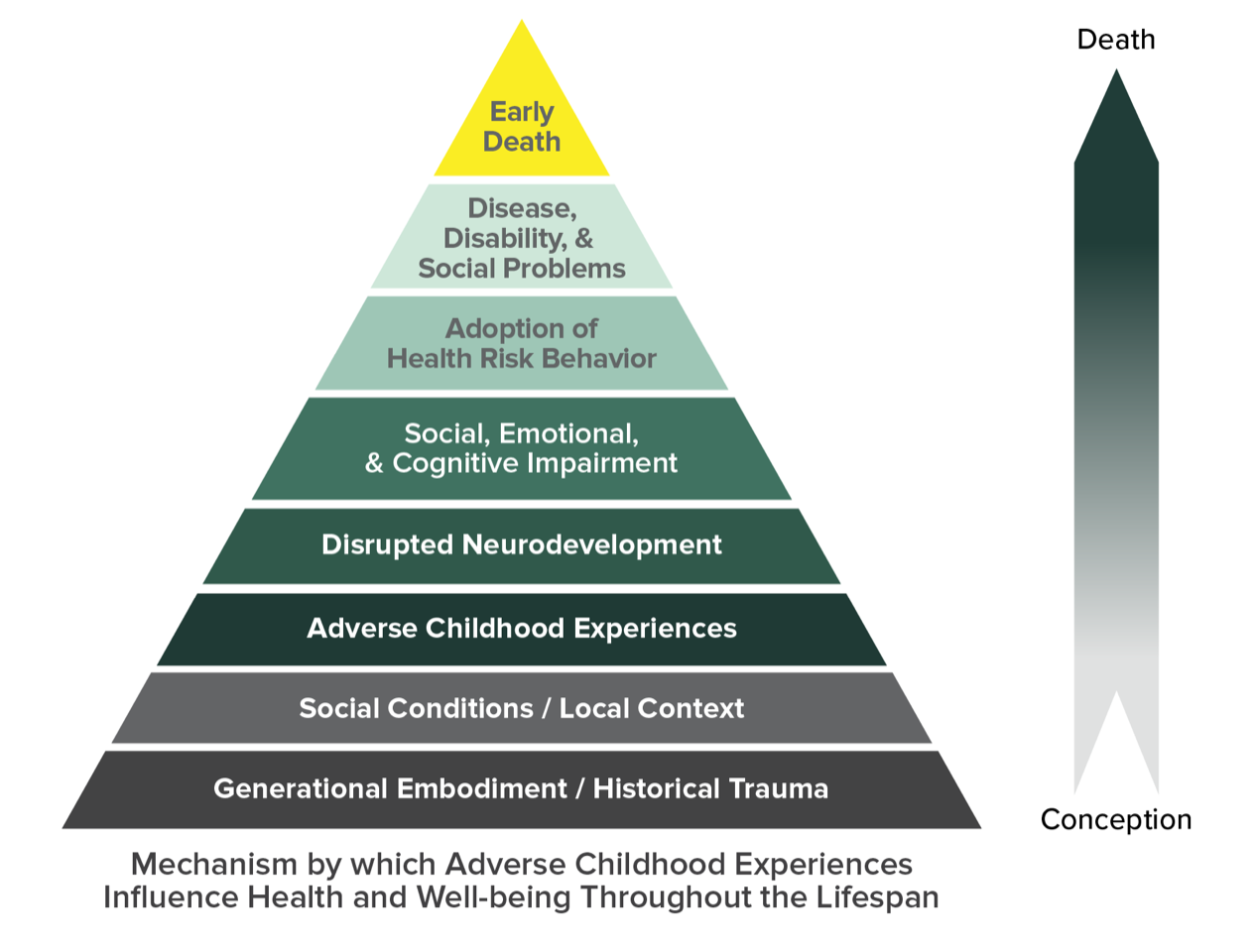
Photo via the CDC
With this much evidence, it is amazing that most physicians do not know about the increased risk and consequently do not use the ACE questionnaire in their practice. In 2020 a peer reviewed article was published that presented the results of a study to try to measure this expected gap (10). This study found that 81% of the primary care physicians were not aware of the ACE questionnaire and only 3% reported using the questionnaire in their practice. This study was limited to a small county in Michigan, but it is at least indicative of a general national situation.
The CDC has stated that understanding and preventing Adverse Childhood Experiences is a strategic focus for public health. In addition, other forms of experiences will need to be evaluated, this will take more research into not just the already identified traumas but also the impact of other experiences such as bullying, experiencing racism, frequent moving, homelessness, food insecurity, death of a parent or family member which can constitute their own traumas or at least can exacerbate the impact of ACE’s. More recently the potential traumatic impact of the COVID-19 Pandemic is a new unknown factor.
A sample questionnaire can be found by following this linkhttp://www.odmhsas.org/picis/TraningInfo/ACE.pdf; it is a questionnaire that is being used by the State of Oklahoma.
The CDC (11) identifies six primary strategies to prevent, reduce or mitigate the impact of ACE’s:
- Strengthening economic supports for families (e.g., earned income tax credits, family-friendly work policies)
- Promoting social norms that protect against violence and adversity (e.g., public education campaigns to support parents and positive parenting, bystander approaches to support healthy relationship behaviors)
- Ensuring a strong start for children (e.g., early childhood home visitation, high quality and affordable childcare, preschool enrichment programs)
- Enhancing skills to help parents and youths handle stress, manage emotions, and tackle everyday challenges (e.g., social emotional learning programs, safe dating and healthy relationship skill programs, parenting skill and family relationship approaches)
- Connecting youths to caring adults and activities (e.g., mentoring and after school programs)
- Intervening to lessen immediate and long-term harms (e.g., through enhanced primary care to identify and address ACEs exposures with screening, referral, and support, victim-centered services, and advancement of trauma-informed care for children, youth, and adults with a history of exposure to ACEs).
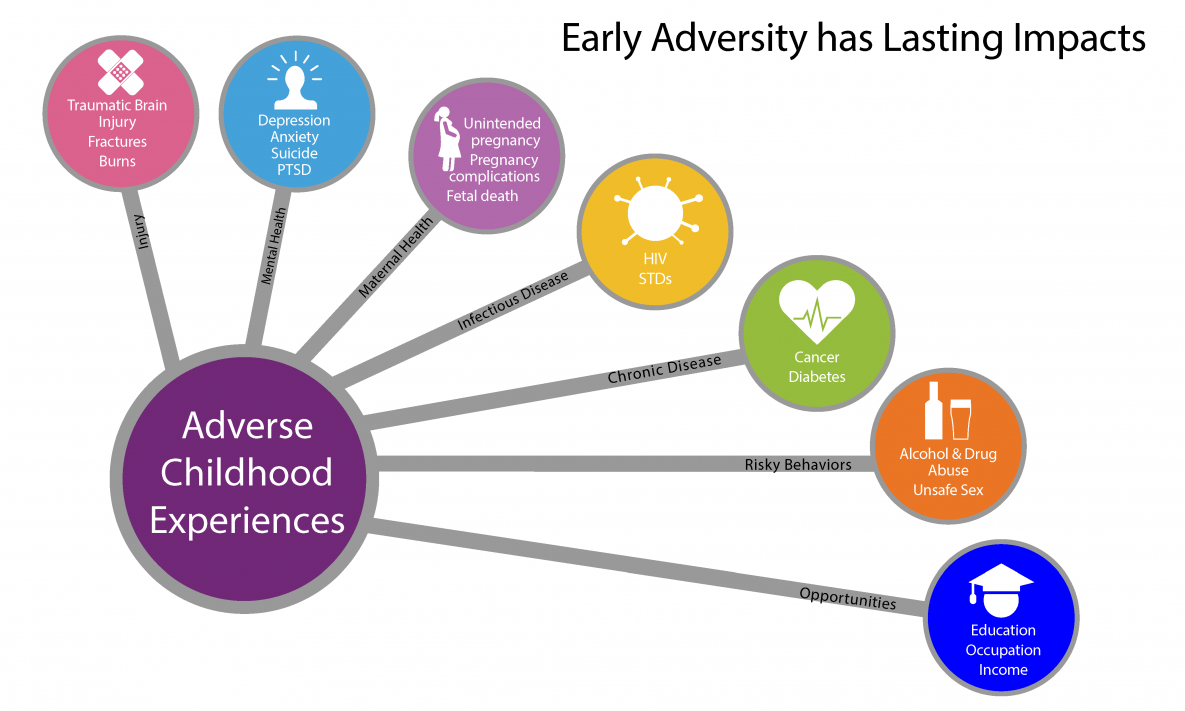
Photo via the CDC
Like almost every other difficult situation government action alone cannot solve the problem; it will take a partnership between, schools, government (local, state, and federal), social services, health services, business and labor, public safety, justice, housing, media, and organizations that comprise civil society such as faith-based organizations, youth-serving organizations, domestic violence and sexual assault coalitions, foundations, and other non-governmental organizations. Some communities like Bayview California have started implementing integrated treatment for children affected by ACEs. Elsewhere the first steps will need to be expanding awareness, implementation of ACE screening, use of proven approaches to reduce the impact of ACEs and the implementation of programs designed to prevent ACEs. Everyone has a role to play in helping to address this public health concern.
References
- Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998 May;14(4)
- Richards M, Wadsworth ME. Long term effects of early adversity on cognitive function. Arch Dis Child 2004 Oct;89(10):922-7.
- Burke NJ, Hellman JL, Scott BG, Weems CF, Carrion VG. The impact of adverse childhood experiences on an urban pediatric population. Child Abuse Negl 2011 Jun;35(6):408-13.
- Kerker BD, Zhang J, Nadeem E, et al. Adverse childhood experiences and mental health, chronic medical conditions, and development in young children. Acad Pediatr 2015 Sep-Oct;15(5):510-7.
- Wade R Jr, Cronholm PF, Fein JA, et al. Household and community-level Adverse Childhood Experiences and adult health outcomes in a diverse urban population. Child Abuse Negl 2016 Feb;52:135-45.
- Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health 2017 Aug;2(8):e356-66.
- Dong M, Giles WH, Felitti VJ, et al. Insights into causal pathways for ischemic heart disease: Adverse childhood experiences study. Circulation 2004 Sep 20;110(13):1761-6.
- Anda RF, Brown DW, Dube SR, Bremner JD, Felitti VJ, Giles WH. Adverse childhood experiences and chronic obstructive pulmonary disease in adults. Am J Prev Med 2008 May;34(5):396-403.
- Brown DW, Anda RF, Felitti VJ, et al. Adverse childhood experiences are associated with the risk of lung cancer: A prospective cohort study. BMC Public Health 2010 Jan 19;10(20):20.
- Stork BR, Akselberg NJ, Qin Y, Miller DC. Adverse Childhood Experiences (ACEs) and community physicians: What we’ve learned. Perm J 2020;24:19.099.
- Centers for Disease Control and Prevention (2019). Preventing Adverse Childhood Experiences: Leveraging the Best Available Evidence. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention.